Complex Regional pain syndrome (CRPS) is a rare condition that combines pain with sensory, autonomic, motor and trophic symptoms. In other words, it’s a cocktail of constant, severe pain with loss of strength and movement, changes in the thickness of the skin and hair, as well as, other sensations like burning or tingling. The symptoms are usually localised to an extremity like the foot or the hand, but sometimes, they tend to spread proximally. In some rare severe cases, it can even spread to the contralateral limb. With all these, the name of CRPS makes more sense: complex (fluctuating multi-pathophysiological factors, all feeding into each other), regional (location of the condition to a regional area) and syndrome (a lot of symptoms at the same time).
Are there types or phases in CRPS?
It used to be called, Algodistrophy, Reflex Dystrophy or Sudeck’s syndrome, but the consensus is now to call it CRPS. It is very important for patients and professionals to know, that CRPS symptoms fluctuate hugely, (even within the same day), so there are no phases or stages of CRPS.
There are 3 types of CRPS. Type 1 (no nerve injury) and type 2 (nerve injury of the large fibers) can be, sometimes, hard to differentiate clinically because the symptoms can be quite similar and/or the nerve conduction studies can be either inconclusive or not able to be done because of pain. The 3rd type of CRPS is called NOS (Not Otherwise Specified). This type is generally reserved for those patients that, either fulfilled the current diagnosis criteria after symptom onset, but they don’t anymore; or those who were diagnosed with an older CRPS diagnosis criteria, but don’t satisfy the current criteria.
Additionally, there are 2 sub-groups of CRPS based on the temperature changes: cold and warm. This refers to the affected limb temperature. Typically, a warm CRPS may develop into a cold CRPS over time; but a cold CRPS rarely transforms into a warm one. Unfortunately, a cold CRPS tends to have a worse prognosis.
The WHO and the HOW
The typical patient may be a middle-age woman 4-6 weeks after having surgery to the foot (like a bunionectomy) or after a wrist fracture. Usually, the intensity of the pain is very high, but it may take a bit longer for other symptoms to appear, delaying the patient from being managed appropriately (i.e. “I’m not a hypochondriac, there is really something not normal here! This pain is excruciating!”). Note that some studies show that vitamin C, early mobilisation and appropriate pain management can prevent CRPS.
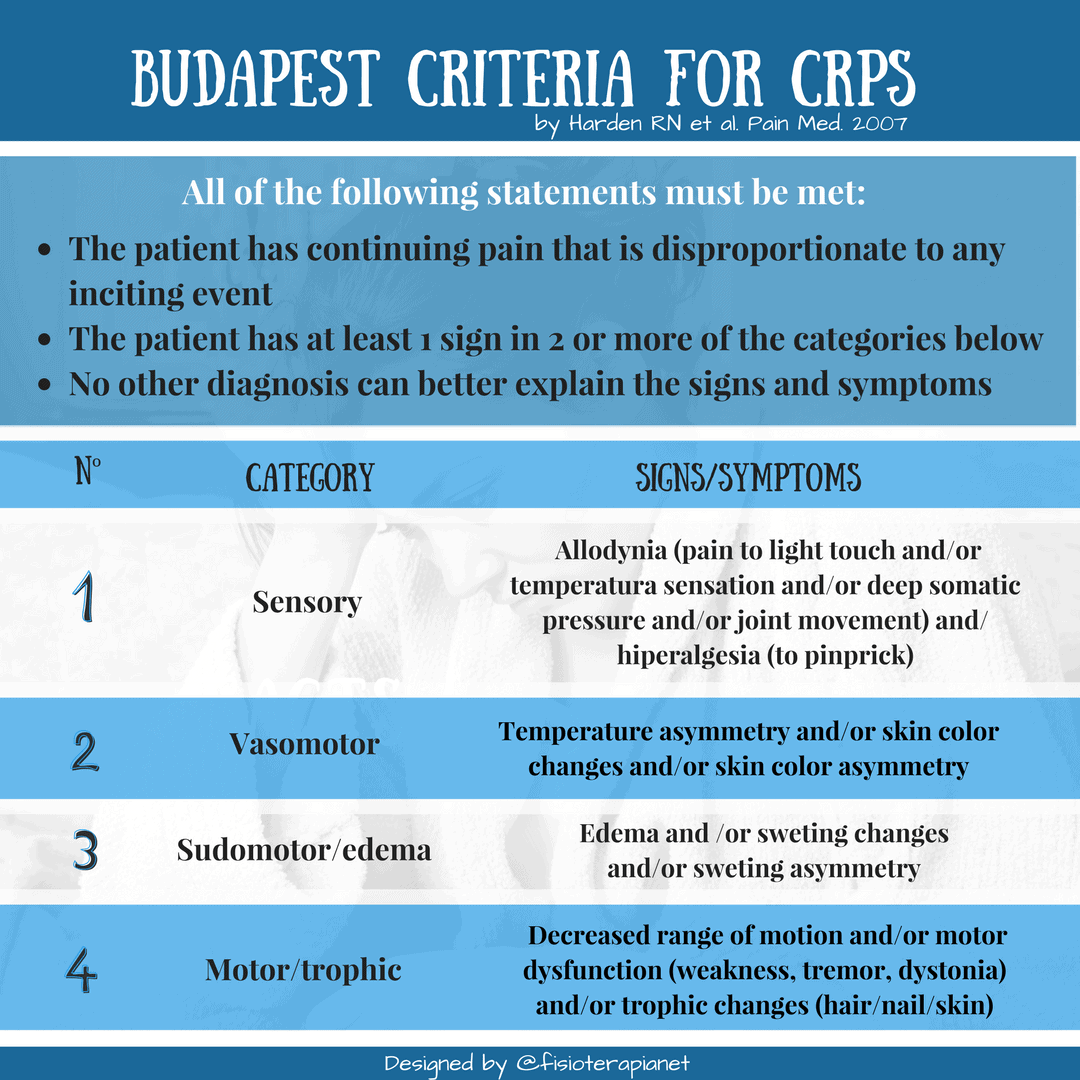
The current (it may change, you never now) diagnosis criteria
The diagnosis of CRPS is primary done by ruling out anything else that is more common and, once this is done, by applying the current diagnostic criteria (currently, it’s called the Budapest CRPS diagnosis criteria, see table attached from Harden et al, 2007). In some cases, the patient has been through a lot of different tests and medications to try to find possible causes and treat the symptoms, before is diagnosed with CRPS. Unfortunately, this may take months. The earlier the diagnosis is confirmed and appropriate treatment is started, the better the chances are for recovery.
The table above says as follow…
All of the following statements must be met:
- The patient has continuing pain that is disproportionate to any inciting event.
- The patient has at least 1 sign in 2 or more of the categories below.
- No other diagnosis can better explain the signs and symptoms.
Categories, signs and symptoms:
1. Sensory: Allodynia (pain to light touch and/or temperatura sensation and/or deep somatic pressure and/or joint movement) and/ hiperalgesia (to pinprick)
2. Vasomotor: Temperature asymmetry and/or skin color changes and/or skin color asymmetry
3. Sudomotor/edema: Edema and /or sweting changes and/or sweting asymmetry
4. Motor/trophic: Decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair/nail/skin).
After looking at the table above, you start to get a clearer picture of the complexity and severity of this condition, where patients have allodynia (cannot even tolerate a gentle blast of wind from an opened window or the air-con of a car), severe pain and, obviously, lack of function. There is even an alteration in body perception and, in severe cases, neglect of the affected limb. In most cases, the combination of the severe and constant symptoms and the difficulty of the diagnosis and management will affects the patient and his/her family emotionally (and financially). They feel helpless and abandoned. If you are reading this, as a patient: you are not alone. If you are reading this as a professional: please don’t abandon them.
There are discussions and disagreements among experts (heard at a conference a couple of years back) about the diagnosis criteria (yes, it may not be perfect, but it’s the only thing we have now) and about having CRPS in other sites rather than the hand or the foot. What Prof. Harden said back then was: “if everything else has been ruled out and the diagnosis criteria has been applied, then it is CRPS”. However, he also acknowledged (and the rest agreed) that the part of “everything else has been ruled out” is very difficult to achieve (time, money, experts, tests…). So… the jury is out!
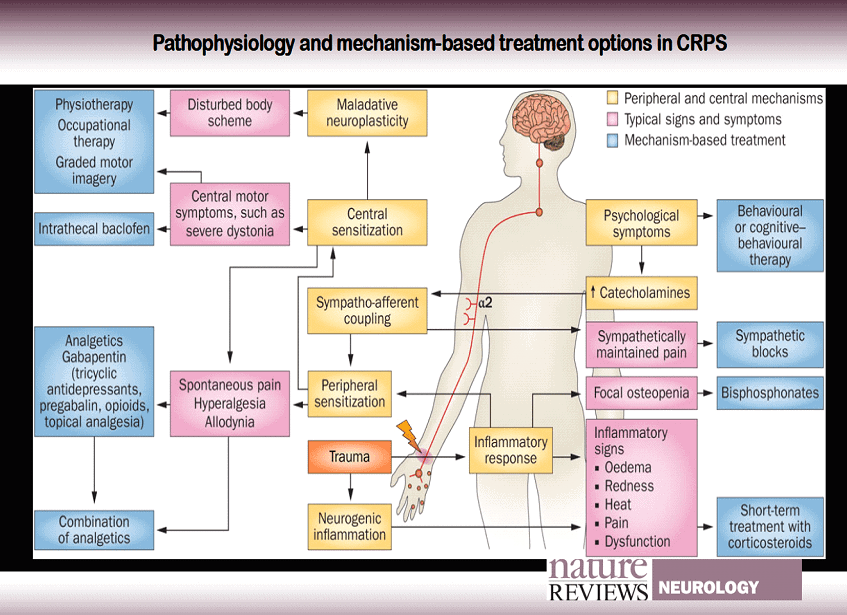
Physiopathology in a nutshell: everything and anything is affected
We could get into the pathophysiological mechanisms of CRPS, but they are complex and, I feel, this blog is not the right platform for discussion, but if you are interested, have a look at the excellent picture below from Janne Gierthmühlen and her team in Kiel (Germany).
What to do if you suspect CRPS
If you suspect your patient has CRPS, then you need to refer him/her to a doctor with experience with CRPS if possible. In some cases, as the waiting lists are soooo long, it may be possible to have a doctor-to-specialist (sorry guys, I wish I could say physio here, but we should not give medical diagnoses) conversation to, if in doubt, start pharmacological treatment.
Luckily, there are treatment guidelines that have been published by US, UK (NICE) and The Netherlands (available in English), apart from Cockhrane, among others, that are quite comprehensive and easy to access. Also, research teams from Prof. Candy McCabe and Lorimer Moseley have published a series of articles that are clinically relevant for physiotherapist and occupational therapist. (Apologies if I have left others out!)
The meds
There is medication available to manage the symptoms, but unfortunately (and possibly due to the complex pathophysiological mechanisms) they work better for some than for others. What it seems to be clear is that WHEN the appropriate medical treatment is started before 6 months of symptoms, the prognosis seems to be better (but not always, a lot to research is needed in this area).
Pharmacological treatment should include (at least in the early stages) steroids and bisphosphonates, as well as others. There are also other medical treatments such as blocks, infusions and amputations that arouse deep discussions and contradictions in the literature. There are a lot of severe side effect from certain medications given intravenous (IV) and, what can we say about the ethical implications of amputation?? The pain can be so severe that patients ask for it themselves!! Unfortunately, there have been described cases, where the CRPS spreads to the contralateral limb… even after amputation!
What we can (YES, WE CAN!) do
There are lots of possibilities regarding the non-pharmacological treatment, but the treatment needs to be individualised to the patient’s pain and allodynia. Techniques such as mirror therapy, desensitisation, right and left discrimination and visualisations can work at a central level. However, education and reassurance should play a vital role in each visit.
Regarding the physical rehabilitation, there are mainly 2 opposite approaches:
⦁ Graded exposure or therapy (GEX)
⦁ Pain exposure physical therapy (PEPT)
Generally speaking, GEX is a soft-but-firm approach, while PEPT is like a military-bootcamp. What I’m trying to say here is that some may enjoy and thrive in a bootcamp, while others may get worse. PEPT removes all coping strategies and mechanisms (so patients and relatives need to be screened to know if they are suitable candidates). Regardless of the approach, the important issue here is that, it has to be the right approach for the patient, the relatives and the therapist.
Lastly, but PRIMARILY, these patients need a multidisciplinary approach, including at least, a pain specialist doctor, a therapist and a psychologist. Please, do not underestimate the power of the brain. The balanced symbiosis created by the team’s contributions can be the perfect method to empower the patients towards self-management and, in some cases, full or partial recovery.
They call themselves “CRPS warriors” and we need to fight with them.
What the future holds…
To my knowledge, there are ongoing investigations looking and phenotyping CRPS, meaning, doing a lot of tests to patients to try to find out a more optimal classification and, ultimately, better pharmacological treatment. There are studies looking at different treatments and approaches… but the reality is that CRPS is rare, so it is not easy!
Para ampliar aun más esta información te recomendamos visitar este sitio web www.rsds.org
Referencias
– Birklein F., Dimova V. Complex regional pain syndrome-up-to-date. Pain Reports. Clinical Updates. 2017.
– Bruehl S, Mailhoefner C, Stanton-Hicks M, Perez RSGM, Vantine JJ, Brunner F, et al. Complex regional pain syndrome: evidence for warm and cold subtypes in a large prospective clinical sample. Pain. 2016;157:1674-1681
– Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;6(4):326-331.
– Harden RN. The diagnosis of CRPS: Are we there yet? Pain 2012; 153:1142-1143
– Harden RN, Maihofner C, Abousssad E, Vatine JJ, Kirsling A, Perez R et al. A prospective, multisite, international validation of the Complex Regional Pain Syndrome Severity Score. Pain. 2017;158:1430-1436.
– Galve-Villa, M, Rittig-Rasmussen B, Mikkelsen LMS, Poulsen AG. Complex Regional Pain Syndrome. Manual therapy 2016;26:223-230
– Gierthmühlen, J. et al. Mechanism-based treatment in complex regional pain syndromes Nat. Rev. Neurol. 2014
– Grieve S, Perez RSGM. Birklein F, Brunner F, Bruehl S, Harden N, et al. Recommendations for a first Core Outcome Measurement set for complex regional PAin syndrome Clinical sTudies (COMPACT). Pain 2017 June; 158(6):1083-1090.
– Goh, EL, Chidambaram S, Ma D. Complex Regional Pain Syndrome: a recent update. Burns & Trauma 2017; 19(5): 5
– Maihofner C, Handwerker HO, Neudorfer B, Birklein F. Patterns of cortical reorganization in complex regional pain syndrome. Neurology 2003; 23;61(12):1702-15
– Perez RS, Zollinger PE, Dijistra P, Thomassen-Hilgersom IL, Zuurmond W, Rosenbrand, KCJ et al. Evidence based gudelines for complex regional pain syndrome type 1. BMC Neurology 2010, 10:20
Spanish version